Contact us at 970-749-4443
Exploring Platelet Rich Plasma and Bone Marrow Concentrate Treatments
Have you heard of platelet rich plasma (PRP) and bone marrow concentrate (BMC) treatments? They are becoming increasingly popular for the treatment of orthopedic injuries. In this article, we will discuss what these treatments are, how they improve healing, and whether or not they can help with your orthopedic injury. #prp
What is Platelet Rich Plasma?
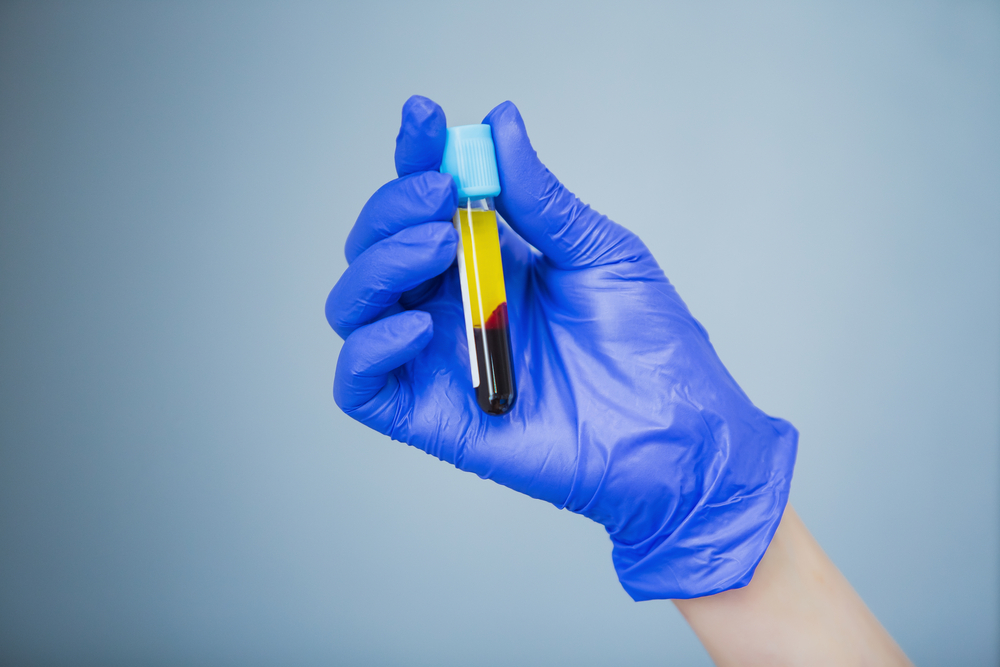
Platelet Rich Plasma (PRP) is a type of therapy that involves extracting a small volume of red blood cells, which are then concentrated in a centrifuge to separate the red blood cells, platelets, and plasma. Depending on the type and location of injury, certain components such as leukocytes (immune cells) may be removed or kept. Once the concentrated mixture is separated (often referred to as “liquid gold”), it’s precisely injected or transplanted into the site of injury. The concentrated platelets found in PRP contain growth factors that help to promote healing and tissue regeneration. PRP injections can be used to treat a variety of orthopedic injuries, including tendonitis, muscle strains, ligament tears, joint pain and arthritis.
How Does PRP Improve Healing?
When injected into an injured area, PRP helps to reduce inflammation while modifying the production of collagen fibers in the affected area. This helps to speed up the recovery process by decreasing pain and improving mobility faster than most traditional treatments alone. In turn, the goal is to improve your quality of life by getting you back to the activities you enjoy the most. Likewise, results often last longer compared to corticosteroid injections without compromising the musculoskeletal tissue.
What is Bone Marrow Concentrate?
Bone marrow concentrate (BMC) is a type of therapy similar to PRP in that it also uses a patient’s own cells as part of the treatment process. In BMC treatments, however, the cells come from bone marrow rather than blood plasma. Unlike PRP injections which only use platelets, BMC injections contain both platelets as well as stem cells which can help with tissue regeneration and healing.
How Does BMC Improve Healing?
Like PRP injections, BMC injections have been shown to reduce inflammation while speeding up recovery times due to its ability to stimulate healthy tissue response in damaged areas. It also has the added benefit of scar reduction due to its ability to promote healthy cell development when injected into an injured area. Additionally, BMC has been shown to be more effective at improving outcomes in certain injuries when compared with other traditional therapies.
Will These Treatments Help With Your Orthopedic Injury?
Platelet Rich Plasma (PRP) and Bone Marrow Concentrate (BMC) treatments offer many potential benefits for those suffering from orthopedic injuries such as tendonitis, muscle strains, partial ligament tears/sprains or mild to moderate arthritis. Both types of treatments have been proven effective at reducing inflammation while promoting healing and restoring mobility faster than traditional treatments alone. If you are considering these types of treatments for your orthopedic injury it is important that you speak with your doctor first so they can evaluate your specific situation before recommending an appropriate course of treatment for you. Please keep in mind that there is no current treatment modality in medicine that is 100% successful in every patient. Some individuals require 2-3 injections before noticing significant improvement. Additionally, your overall health and lifestyle will impact the quality of platelets and cells extracted. We are happy to discuss the best treatment options for you.
What You Need to Know About PRP Quality and Underlying Medical Conditions, Medications, and Lifestyle Factors
Platelet-rich plasma (PRP) therapy is a regenerative medical treatment that has been used for many years to treat various chronic pain conditions. It is based on the idea of using the body’s own natural healing powers to assist in repair of damaged tissue and reduce inflammation. In recent years, PRP has become increasingly popular as an alternative treatment option for many common medical conditions. In this article, we will discuss some of the medical conditions that can impact the effectiveness of PRP treatments, as well as which patients respond best to this type of therapy.
Medical Conditions That Impact PRP Outcomes:
The current physiological status of the patient, or how efficiently the machine (or human body) is functioning, is a key consideration when evaluating the effectiveness of the treatment. Certain medical conditions can make it difficult for the body to absorb platelet-rich plasma or make it hard for the body to produce enough platelets. For example, people with chronic conditions such as poorly controlled diabetes, peripheral vascular disease, uncontrolled hypertension (high blood pressure), or heart failure may not be able to respond as effectively to PRP treatments since their bodies are already impacted with diminished circulation and reduced platelet quality. Additionally, people with autoimmune disorders such as lupus or rheumatoid arthritis may be unable to produce enough platelets for successful PRP treatments. Finally, certain medications can decrease platelet production and/or function. A few examples include NSAID’s, selective serotonin reuptake inhibitors (SSRI’s), antihistamines, antibiotics, and tricyclic antidepressants.
Diet and Lifestyle Factors That Impact PRP Outcomes:
Nutrition plays a large role in the quality of platelets your body produces. Diets high in processed foods, sugar, simple carbohydrates, and omega 6 fatty acids (found in industry seed oils) can impact platelet activation, production, and aggregation. All of these factors are important in the overall quality of PRP and in turn, your natural healing response. Additionally, excessive alcohol consumption and tobacco use can reduce the platelets response to thrombin and collagen, making them less effective. Lastly, physical and mental stress induces a spike in hormones such as adrenalin, noradrenaline, and serotonin, which impacts the platelets sensitivity to thrombin, factor release, and aggregation. High intensity exercise prior to your procedure can induce physical stress and potentially impact your treatment.
Patients Who Respond Best To PRP Treatments:
Similarly to invasive surgical outcomes, individuals who strive to live a healthy lifestyle by incorporating routine exercise, a well-rounded diet low in processed foods, and adequate sleep will respond best. However, our patients with multiple underlying medical problems are at higher risk for surgical complications and oftentimes minimally invasive procedures can provide pain relief and improved functionality. Utilizing precision medicine, we strive to optimize all modifiable factors prior to treatment for optimal results.
In conclusion, there are several medical conditions, medications, and lifestyle factors that can affect how effective a patient’s response is when undergoing a course of platelet-rich plasma (PRP) therapy. Despite all this, there are still many patients who respond very positively when undergoing courses of treatment involving PRP therapy; those suffering from chronic pain conditions such as tendinitis or bursitis often see great improvement in their symptoms after undergoing one or multiple rounds of treatment while athletes can use it help improve performance during competitions as well as reducing inflammation afterward. When considering PRP, we would highly suggest seeking out physicians who understand the relationship between platelets and other medical/lifestyle factors to ensure the best possible outcome.
Kuffler DP. Variables affecting the potential efficacy of PRP in providing chronic pain relief. J Pain Res. 2018 Dec 21;12:109-116.
Barkin RL, Fawcett J. The management challenges of chronic pain: the role of antidepressants. Am J Ther. 2000;7(1):31–47.
George JN. Platelets. Lancet. 2000;355(9214):1531–1539.
Ahmed Y, van Iddekinge B, Paul C, Sullivan HF, Elder MG. Retrospective analysis of platelet numbers and volumes in normal pregnancy and in pre-eclampsia. Br J Obstet Gynaecol. 1993;100(3):216–220.
Mukamal KJ, Massaro JM, Ault KA, et al. Alcohol consumption and platelet activation and aggregation among women and men: the Framingham Offspring Study. Alcohol Clin Exp Res. 2005;29(10):1906–1912.
Belch JJ, McArdle BM, Burns P, Lowe GD, Forbes CD. The effects of acute smoking on platelet behavior, fibrinolysis and haemorheology in habitual smokers. Thromb Haemost. 1984;51(1):006–008.
Warkentin TE, Kelton JG. Temporal aspects of heparin-induced thrombocytopenia. N Engl J Med. 2001;344(17):1286–1292.
de Lorgeril M, Renaud S, Mamelle N, Salen P, et al. Mediterranean alpha-linolenic acid-rich diet in secondary prevention of coronary heart disease. Lancet. 1994;343(8911):1454–1459.
Sudic D, Razmara M, Forslund M, Ji Q, Hjemdahl P, Li N. High glucose levels enhance platelet activation: involvement of multiple mechanisms. Br J Haematol. 2006;133(3):315–322.
